Improving prosthetic limbs for children
Mechanical and aerospace engineering (MAE) assistant professor Jonathon Schofield, neurobiology, physiology and behavior (NPB) associate professor Wilsaan Joiner and their team are working to develop better and more functional prosthetic devices for children.

For some children born without fully-formed limbs, prosthetic devices can be helpful, and many are prescribed their first prosthetic when they are 6-18 months old. 35-45% eventually decide not to wear a device either because it’s uncomfortable, doesn’t offset the function they would otherwise have, or they don’t have a sense of loss the way an adult who lost a limb would. These children grow up to lead happy, healthy and functional lives without prosthetics, but Schofield wants to give them better options if they choose to wear one.
“We think there might be a pathway to providing more meaningful, functional and useful devices for children who are affected with limb differences to consider,” he said. “It’s about providing something that is hopefully useful in some capacity; something that can help them integrate and participate similar to their peers in many ways.”
For Joiner, who studies how the brain controls the limbs and movement, the behavior of muscles in the absence of a limb is closely tied to how a body might better-interact with a prosthetic device.
“A question that hasn’t yet been addressed is: how does the brain deal with a limb that was never there to begin with?” he said.
Reading Signals
In a new three-year NSF-funded project, Schofield, Joiner and collaborators at Shriners Hospital in Sacramento will begin learning what’s possible. The first step is figuring out what each child’s affected muscles can do.

“For children who have never operated an intact limb, we really don’t completely understand how their muscles operate, and we don’t understand how we can use that muscle activity to drive more advanced prostheses,” Schofield explained.
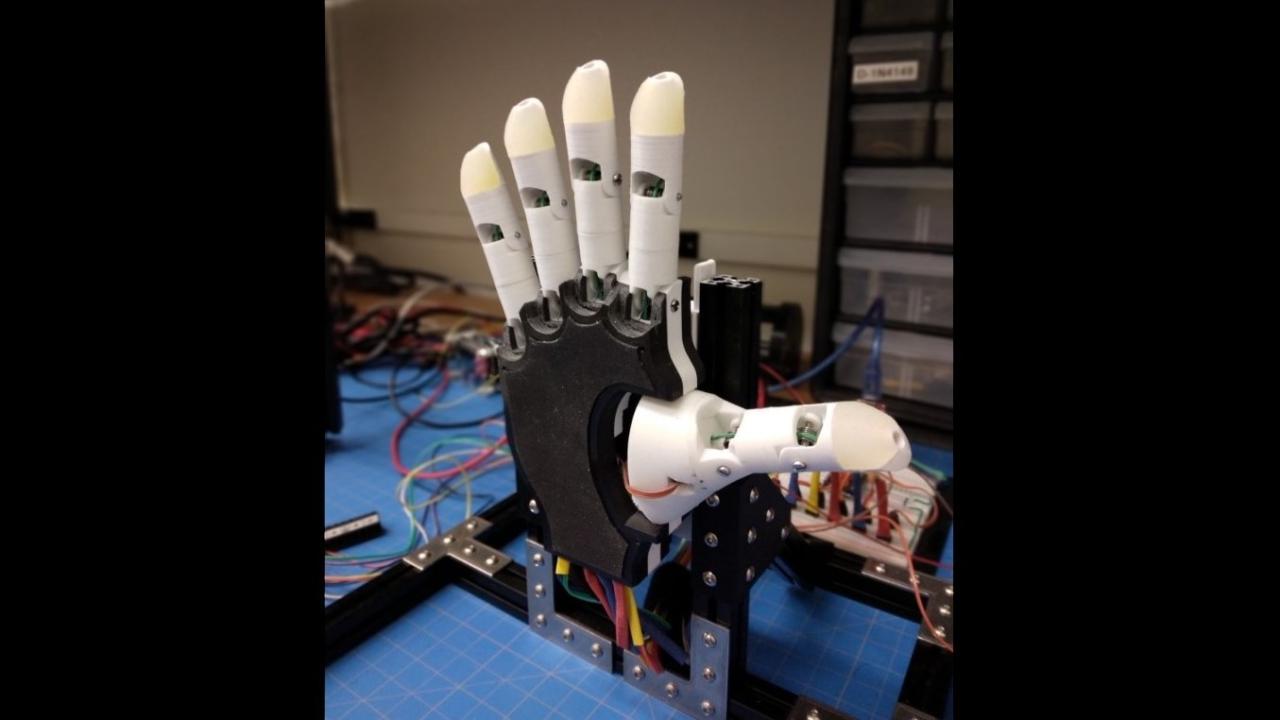
To find out, the team will ask patients to imagine performing actions such as pointing, pinching or making a fist with their missing limb and record muscle signals at the affected site using skin-based muscle sensors and ultrasound imaging. They will then use machine learning to read these signals, recognize the patient’s intention and explore what types of movements are possible.
“Although individuals have never had an intact hand on the affected side, we have a lot of preliminary data to suggest that we can pick out differences in their muscle activity when we asked them to do something like a power grip vs. pointing vs. pinching,” said Schofield. “It appears that there is some sort of representation of the missing hand, even though it was never really there. That in itself is some very exciting preliminary evidence that I think we’re going to really flesh out with this grant.”
The team will also train children how to use their affected muscles using a video game. The game asks children control a spaceship by imagining making different movements with their missing limbs. It then measures the activity of their affected muscles and uses this to control the ship.
“It’s prompting them to think about using their missing hand in different ways,” said Schofield. “We want to explore how they can learn and train and what differences in performance we would see as a result.”
A First Step
Schofield and Joiner are thankful to be working on the project with collaborators who bring multi-faceted expertise in neurobiology and pediatric medicine to this problem.
"Approaching this issue effectively requires a fairly broad range of skills and expertise,” said Joiner. “Coupling the understanding of the motor system and learning with engineering techniques and clinical measures and assessments enhances our ability to conduct truly translational research"
“This is a multi-dimensional problem that’s not exclusive to the engineering,” said Schofield. “It’s not something that could be done by just our lab or just doctors. It works because we are all in it together.”
Schofield thinks this is the first of many projects for the team in this area, and stresses the importance of evaluating their work as it progresses to make sure it’s making a real difference in children’s lives. He acknowledges that better prosthetics may not ultimately affect rejection rates, but he wants to make sure those that do wear them have a better and more meaningful experience.
“Some of these systems work very well and have a huge amount of promise for adults, so we see this as a study that allows us to start taking these technologies and transition and translate them to use for children,” he said.
More on this Research
- Learn more about Schofield's lab.
- Read the UC Davis Health newsroom article: Cross-campus collaboration leads to ‘smart prosthetics’ for amputee patients
