UC Davis engineering projects fight COVID-19
Originally posted by the UC Davis College of Engineering.
With new seed grants from the UC Davis Office of Research’s COVID-19 Research Accelerator Funding Track (CRAFT), three teams of UC Davis engineers are applying their expertise toward the pandemic response to help people become safer, healthier and better-tested.
Mechanical and aerospace engineering (MAE) professor and chair Cristina Davis and chemical engineering (CHE) faculty Priya Shah, Karen McDonald and Roland Faller received $25,000 project awards for research that rapidly generates new insights about COVID-19, while biological and agricultural engineering (BAE) professor Gang Sun received a $5,000 small award to apply current research to the pandemic response. These proposals were chosen out from more than 100 applications and were awarded with the expectation that these projects will lead to larger collaborations.
Using Breath to Predict COVID-19 Cases
MAE professor Cristina Davis and her team are using portable devices that capture people’s breath to look for chemical and biological markers, known as biomarkers, to identify and predict the severity of COVID-19 infections.
Davis’ lab produces portable chemical sensing devices that record chemicals from the air or a person’s breath using mass spectroscopy. As part of an ongoing project with professor Nick Kenyon and associate professor Michael Schivo at the UC Davis Medical Center, the team had been conducting a clinical study with these devices to try to find early, asymptomatic biomarkers for the flu. When the pandemic began, the shift to COVID-19 was an obvious one.
“We just happened to be at the right place and the right time to be able to help,” said Davis. “Now that you have people who are coming into the emergency room with COVID-19 infections, you potentially can use these same processes and approaches to look at a different viral infection.”
The campus grant will allow them to expand their clinical study to patients who test positive for COVID-19, but do not have severe enough symptoms to be admitted to the hospital. These patients will be sent home with these devices to record their breath 1-2 times per day as the illness progresses.
Davis hopes to use these data to find biomarkers that predict the severity of the illness, as well as new biomarkers that could help doctors find drugs to help treat it.
“This project is a bit exploratory—we don’t know what we’re going to find,” she said.
Making Proteins for Serological Tests
CHE assistant professor Priya Shah and professors Karen McDonald and Roland Faller are working to find new ways to produce COVID-19 spike proteins for serological tests for antibodies.
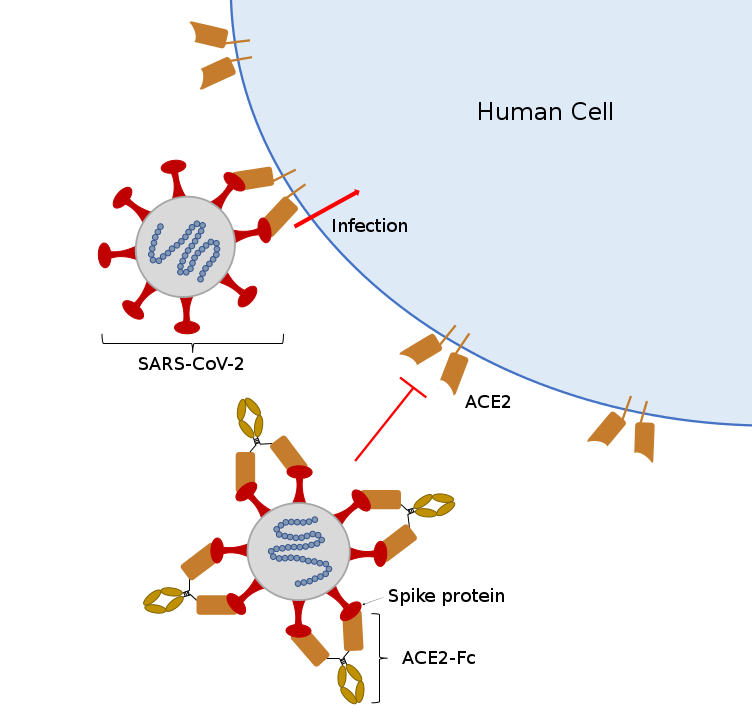
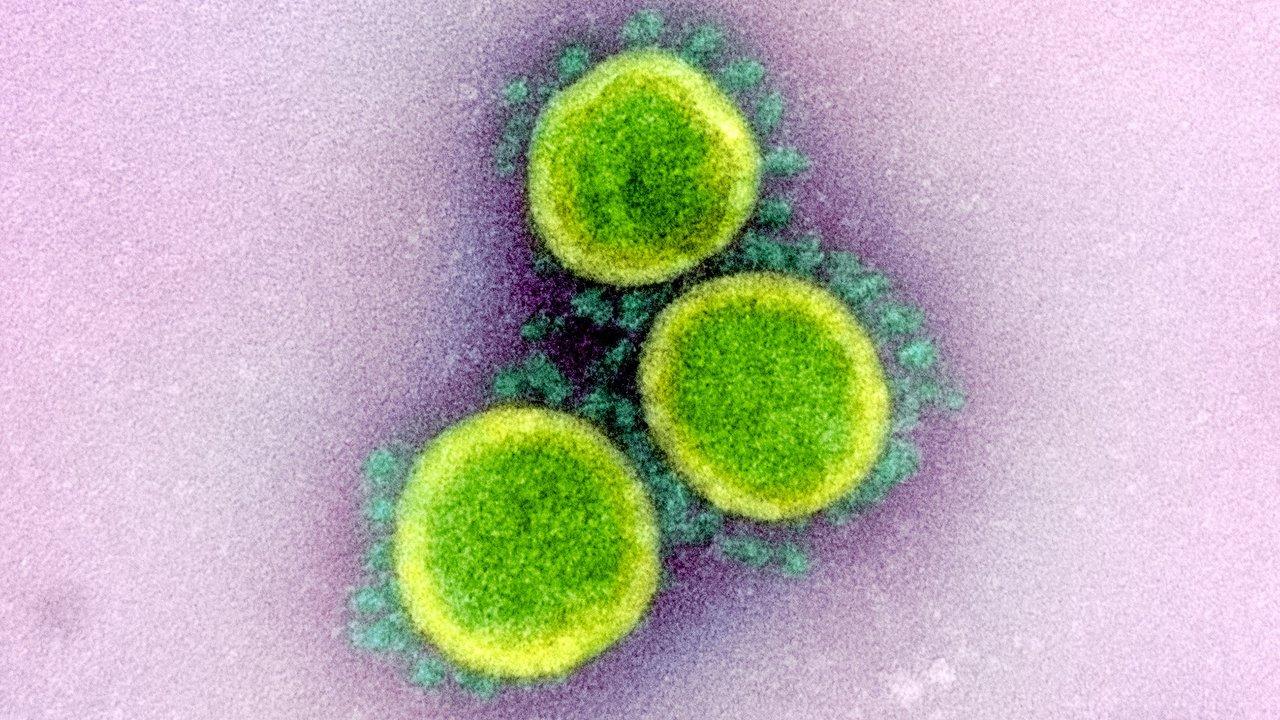
Spike proteins are the little spikes that surround a coronavirus and make it look like a sun. These proteins are the virus’ tool for binding with cells. During an infection, antibodies go after these proteins to stop them from binding to cells. If a sample has these antibodies, they will identify and bind to the protein and the serological test will come back positive.
To reach herd immunity—an important step toward safely re-opening the country—Johns Hopkins University estimates that 70% of the population needs to have COVID-19 antibodies, making regular serological testing necessary for millions of people. This means producing millions, if not billions, of serological tests, which requires an even larger number of spike proteins.
However, because these proteins are glycosylated, or modified by sugars, they are difficult to produce in bacteria, but ideal for living cells. This is where Shah and McDonald come in. With expertise in producing proteins by regulating mammalian and plant cells, respectively, they hope to modify their existing work to figure out the fastest and most efficient way to make COVID-19 proteins.
Faller’s group, known for its computer simulations of glycosylated proteins, will help inform McDonald and Shah’s studies and find the best production strategies for making COVID-19 proteins for tests.
“This is a great example of where microbiology and virology meet chemical engineering,” said Shah. “I think it really nicely brings together multiple labs in the chemical engineering department to make progress on an important problem.”
Reusable Antiviral Face Masks
BAE professor Gang Sun and his team are testing new antiviral chemicals for reusable face masks to protect hospital workers, first responders and essential employees on the front lines of the pandemic.
Sun is a renowned researcher in textiles and fibers and has a legacy of innovation in personal protective equipment. His lab developed an antiviral fabric to combat the original SARS outbreak in 2002 that could be reused by recharging the chemicals with chlorine bleach between uses.
However, the chlorine-rechargeable chemicals aren’t ideal because some are allergic or bothered by the smell. So, Sun’s team pioneered a new solution in 2018 using Vitamin K derivatives to produce antiviral reactive oxidant species. These chemicals offered a side effect-free alternative to chlorine and could be similarly recharged using indoor lighting.
With the CRAFT grant, Sun’s team will see how well they can apply these chemicals to cotton, since their initially tests were done with nanofibers, which have a much larger surface area.
“We have to solve whether we can evenly and controllably apply this onto the surface of the cotton fabric, and also demonstrate that those agents on that cellulose—the cotton—still possesses the same function,” he said.
If successful, Sun hopes to work with medical centers and industry partners across the country to bring this technology to the emergency room.
“Wearing these face masks might be a safe option until the vaccine comes out, so hopefully we can have these types of materials that are useful for battling infections.”
